Dr. David O’Brien | Widening Participation and Outreach Champion | Lincoln Medical School
Dr. Gill Garden | Director of Clinical Skills | Lincoln Medical School
Dr. Ahmet Durgungoz | Digital Education Developer | Lincoln Medical School
The University of Lincoln had to switch to remote teaching during the Covid-19 outbreak, offering Clinicians and the Digital Education Developer the opportunity to collaborate in piloting various ways of delivering learning modules online. As a Medical School, one of our challenges was delivering face-to-face Clinical Skills teaching in an online learning space. This has proven to be challenging since practical and face-to-face interactions are usually a must-have for this area of medicine. We wanted to go beyond uni-directional online lectures, producing a more engaging, high quality, and interactive online student learning experience (Turnbow and Roth 2017). To develop an effective online lesson in a short period of time during a pandemic, the following steps were needed:
- We needed to understand what digital tools we could make use of and their limitations.
- We needed to have a good grasp of the content of the module to formalize what kinds of tools we could use.
- We needed to work collaboratively in an agile way to ensure we had a common understanding of the product we wanted to create, which is an important aspect of instructional design (Lo and Dale 2009).
- As a team, we needed to discuss how we could provide an engaging online experience without losing the quality of the content
- Finally, we needed to have an emphatic approach as to what to expect from the students in a pandemic, so as not to set out unrealistic and challenging targets for them (Helmich, Bolhuis et al. 2011).
The first two modules we designed were based on cardiovascular history-taking and pneumonia. We employed a case-based learning approach to develop the lessons. To increase the engagement of the students and the quality of the learning experience, we employed a blended learning approach (McLean 2016). To match the pedagogy to the result, we made use of various digital software.
The lesson package included three audio recordings of the clinicians role-playing a patient and a doctor. This allowed us to replicate a realistic patient-doctor interaction. The audio recordings were used, along with avatars or animated characters, as can be seen in the below figures. It was important to use multimedia scenarios, as this has a significant impact on making the online lesson more engaging (Herbst and Chazan 2015). An example of this can be seen below:

Figure 1. A scene from a Doodle that illustrates the background of the patient’s problem
Figure 2. A Doodle that represents doctor-patient communication in a hospital setting
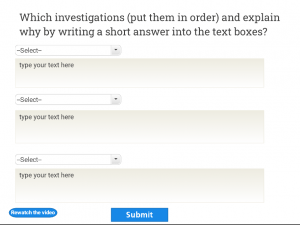
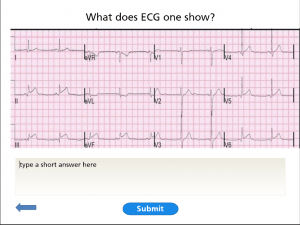
To be able to mimic face-to-face lectures and teach the basic core elements of the lesson, we recorded four micro-lectures. The aim of using several micro-lectures rather than one long recording was to keep the students engaged with the lesson, as it is reported that drop-out rates dramatically increase with longer videos (Kim, Guo et al. 2014). Another aim of preparing ‘bite-sized’ lecture recordings was to test students’ knowledge of the topic, as test-enhanced learning and repetitive testing are found to be effective in enhancing clinical knowledge (Larsen, Butler et al. 2008). Thus, a series of open-ended, drag-drop, multiple-choice questions were embedded after each lecture recording or the audio recordings. This was to enable the students to test their level of understanding before completing the whole lesson in order to minimize cognitive overload (Van Merriënboer and Sweller 2010).
Figure 3. An example of a ranking and an open-ended question used for sense checking
Figure 4. An open-ended question about assessing the patient’s situation
Figure 5. An example of a Multiple Choice Question
Whilst the quality of the content is obviously of paramount importance, other critical aspects in developing such an online learning environment are ensuring that the learning package is accessible with good guidance and is well supported throughout the module (McAndrew, Farrow et al. 2012). Ensuring accessibility and clarity is not only helpful for the students but also minimizing our workload.
All in all, we believe that working collaboratively (Medical Teachers and the Digital Education Developer) on this project has proven to be a successful experiment and one which will hopefully result in further similar opportunities for online teaching and learning in the future.
References
Helmich, E., et al. (2011). “Early clinical experience: do students learn what we expect?” Medical Education 45(7): 731-740.
Herbst, P. and D. Chazan (2015). “Studying professional knowledge use in practice using multimedia scenarios delivered online.” International Journal of Research & Method in Education 38(3): 272-287.
Kim, J., et al. (2014). Understanding in-video dropouts and interaction peaks inonline lecture videos. Proceedings of the first ACM conference on Learning@ scale conference.
Larsen, D. P., et al. (2008). “Test‐enhanced learning in medical education.” Medical Education 42(10): 959-966.
Lo, L. S. and J. M. Dale (2009). “Information literacy “learning” via online tutorials: A collaboration between subject specialist and instructional design librarian.” Journal of Library & Information Services in Distance Learning 3(3-4): 148-158.
McAndrew, P., et al. (2012). “Adapting online learning resources for all: planning for professionalism in accessibility.” Research in Learning Technology 20(4): 345-361.
McLean, S. F. (2016). “Case-based learning and its application in medical and health-care fields: a review of worldwide literature.” Journal of Medical Education and Curricular Development 3: JMECD. S20377.
Turnbow, D. and A. Roth (2017). Engaging learners online: Using instructional design practices to create interactive tutorials. Distributed learning, Elsevier: 123-134.
Van Merriënboer, J. J. and J. Sweller (2010). “Cognitive load theory in health professional education: design principles and strategies.” Medical Education 44(1): 85-93.